Uterine Fibroids/Prolapse
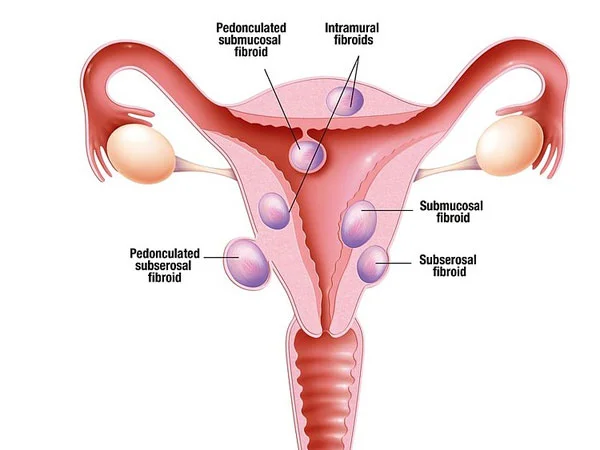
Uterine fibroids are noncancerous growths that develop in the muscular wall of the uterus. They are also known as leiomyomas or prolapsed myoma. Prolapsed fibroids are very common, with up to 70% of women developing them during their lifetime. Fibroids can vary in size, number, and location within the uterus.
Symptoms
While some women with fibroids may not experience any symptoms, others may experience symptoms like,
- Heavy or prolonged menstrual bleeding
- Pelvic pain or pressure
- Frequent urination
- Difficulty emptying the bladder
- constipation, or backache.
Fibroids may also contribute to infertility or difficulties during pregnancy and childbirth.
The exact cause of uterine fibroids is unknown, but it is believed that hormones such as estrogen and progesterone play a role in their development and growth. Risk factors for fibroids include being of reproductive age, African American ethnicity, having a family history of fibroids, and obesity.
Treatment:
Treatment options for fibroids depend on the severity of symptoms and the size and location of the fibroids. Treatment options may include
- Medications to control symptoms
- Hormonal therapy to shrink the fibroids
- Surgical interventions such as myomectomy or hysterectomy.
Prolapse
Prolapse is a medical condition that occurs when an organ or tissue in the body falls or slips out of its normal position. Prolapse can occur in different parts of the body, including the pelvic area, such as the uterus, bladder, or rectum, as well as the organs of the gastrointestinal tract and the anus.
Pelvic organ prolapse is a common condition that affects many women, particularly those who have given birth, gone through menopause, or have a history of pelvic surgery.
Prolapse
- Feeling of pressure or fullness in the pelvis
- Discomfort or pain during sex
- Urinary incontinence
- Difficulty having a bowel movement.
Treatment
Treatment for prolapse depends on the severity of the condition and the type of prolapse. Mild cases of pelvic organ prolapse may not require treatment, while more severe cases may require surgical intervention. In some cases, lifestyle modifications such as pelvic floor exercises or weight loss may be recommended.
